Dentistry
The Connection Between Gum Health and Systemic Inflammation
Key Takeaways
- Gum disease is closely linked to systemic inflammation, which can affect overall health.
- Maintaining good oral hygiene can reduce the risk of chronic diseases.
- Regular dental checkups are essential for early detection and prevention.
Table of Contents
- Understanding Gum Disease
- The Role of Inflammation
- Systemic Health Implications
- Mechanisms Linking Gum Disease and Systemic Inflammation
- Preventive Measures
- Conclusion
Oral health is often underestimated in its importance to overall well-being. Still, scientific research increasingly shows that your gums play a critical role in more than just a healthy smile. The link between gum health and systemic inflammation extends far beyond the mouth, connecting oral care to the risk of chronic diseases that impact the heart, lungs, and metabolic system. If you’re searching for comprehensive oral care, consider finding a holistic periodontist Greenwich, CT, who can address both your dental and systemic health needs.
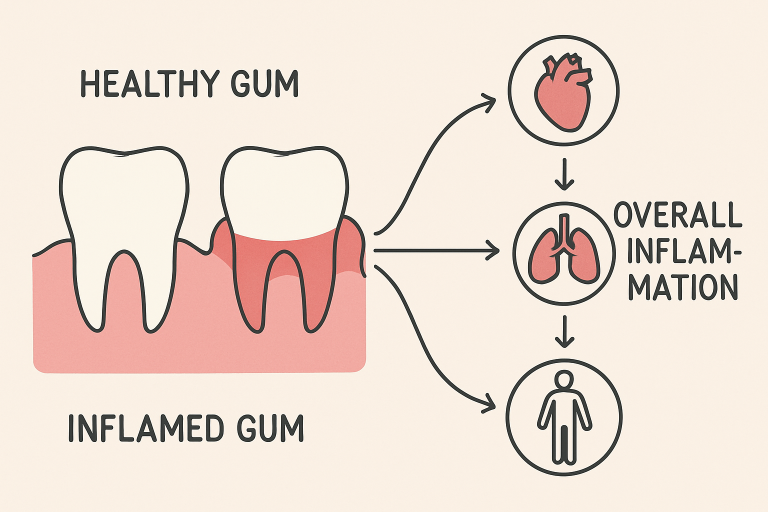
Inflammation is a key biological response to infection and injury, and when it becomes chronic, it drives diseases throughout the body. Gum disease (characterized by redness, swelling, and bleeding) can trigger a chain reaction that escalates inflammation beyond your mouth. By understanding the connection between gum health and systemic inflammation, you can make informed choices about your oral hygiene habits and preventive care.
A holistic approach to dental care not only targets symptoms in your gums but also considers how they may affect your entire body. Early intervention and preventive practices are essential for protecting both your oral health and your long-term vitality. Periodontists and integrative dental professionals are increasingly recognizing this synergy, and the evidence supporting their approach continues to grow.
As you explore how healthy gums are intertwined with overall inflammation, it’s important to recognize the far-reaching impact on chronic conditions such as heart disease, diabetes, and respiratory health. Maintaining your oral health is one of the most accessible ways to lower your risk of systemic illness.
Understanding Gum Disease
Gum disease, or periodontal disease, is a prevalent chronic inflammatory condition affecting the tissues that surround and support your teeth. The earliest stage, gingivitis, manifests as swollen, tender gums that may bleed during brushing or flossing. If left untreated, gingivitis progresses to periodontitis, where the gums recede and infection can damage the jawbone and connective tissue, ultimately leading to tooth loss.
Poor oral hygiene, smoking, genetic predisposition, certain medications, and underlying health issues can all contribute to gum disease. The disease process starts with the accumulation of bacterial plaque—a sticky, invisible film that forms on teeth. As plaque hardens into tartar, the inflammation worsens, making it easier for bacteria to invade gum tissue.
The Role of Inflammation
Inflammation is the body’s defense mechanism, designed to control infection and promote healing. However, with gum disease, the body’s immune response becomes prolonged and exaggerated. When the immune system detects persistent oral bacteria, it sends out inflammatory mediators to eliminate them. Over time, chronic exposure to these signals leads to tissue destruction rather than healing, allowing oral microbes to persist and the inflammation to spread beyond the gums.
The consequences of unresolved gum inflammation are not isolated to the mouth. Bacteria and inflammatory mediators can enter the systemic circulation, affecting distant organs and contributing to widespread inflammation. Chronic, low-grade inflammation is a recognized risk factor for many major diseases, underscoring the importance of gum health.
Systemic Health Implications
Extensive research underscores the connection between poor gum health and systemic disease. Chronic gum inflammation has been linked to a range of serious health issues:
- Cardiovascular disease: Individuals with periodontitis are at higher risk of arterial plaque buildup, heart attacks, and strokes. The American Heart Association reports that oral bacteria may help trigger the narrowing of arteries (atherosclerosis) and the formation of clots, which can disrupt blood flow.
- Diabetes: Gum disease complicates blood sugar regulation, and people with diabetes are more vulnerable to gum infections. This relationship means that controlling one condition helps improve the other, creating a feedback loop between diabetes management and periodontal health.
- Respiratory infections: Harmful oral bacteria can be aspirated into the lungs, leading to diseases such as pneumonia, especially among the elderly or immunocompromised.
Mechanisms Linking Gum Disease and Systemic Inflammation
The relationship between oral and systemic inflammation is based on several interconnected biological mechanisms:
- Bacterial translocation: When gums are inflamed, they become porous, allowing oral pathogens to enter the bloodstream. These bacteria can spread to other parts of the body, where they may cause further infection and inflammation.
- Immune system activation: The body’s attempt to fight off gum infections leads to the continuous release of inflammatory cytokines and mediators, contributing to an overactive immune response throughout the body.
- Elevated inflammatory markers: Blood tests often show that people with active periodontal disease have increased levels of C-reactive protein (CRP) and other markers of systemic inflammation, which correlate with cardiovascular and metabolic risk.
Emerging Research and Clinical Evidence
Recent studies emphasize the importance of managing periodontal disease for systemic health. For example, individuals receiving intensive periodontal therapy have been shown to experience reductions in systemic markers of inflammation and cardiovascular risk factors. As our understanding of these interconnections evolves, integrating dental and medical care becomes increasingly critical for comprehensive wellness.
Preventive Measures
Protecting your gums is one of the most practical ways to control systemic inflammation. Here are effective strategies to safeguard both your oral and overall health:
- Brush your teeth at least twice daily with fluoride toothpaste, focusing on the gumline.
- Floss or use interdental brushes to clean between teeth and below the gums.
- Schedule regular dental visits for professional cleanings and inspections to catch early signs of disease.
- Avoid all tobacco products, as they can accelerate gum deterioration and systemic inflammation.
- Adopt a balanced, nutrient-rich diet to strengthen immune function and support tissue repair.
Healthy lifestyle habits, including stress management and regular exercise, further enhance immune function and reduce the likelihood of chronic inflammation.
Conclusion
Maintaining optimal gum health is a powerful way to reduce your risk of chronic diseases linked to systemic inflammation. By combining diligent home care with professional dental support, you can protect both your smile and your long-term wellness. Understanding and acting on the mouth-body connection is an investment in your future vitality.